MADISON — Wisconsin’s most vulnerable will have to wait at least a couple more weeks for the COVID-19 vaccine.
While there are numerous logistical reasons for the delayed distribution to the state’s nursing homes, legislative sources say the Evers administration has complicated the problems by its failure to communicate.
‘Poor planning’
Some 2.9 million vaccine doses in the first national wave of distributions shipped out on Sunday, with the first vaccinations underway at priority health points, including Wisconsin hospitals. But it could be the end of the month, at the earliest, before the vaccine distribution process begins at Wisconsin’s 360 nursing homes. Meanwhile, at least four other states are set to begin administering the vaccine at long-term care facilities this week.
The Evers administration said it waited until it had a clear idea of how many doses the state would receive from vaccine makers Pfizer and Moderna.
But there’s more to it than that. Legislative insiders tell Wisconsin Spotlight that contrary to Gov. Tony Evers’ pronouncements that his administration has long been gearing up for vaccine distribution, it wasn’t fully prepared when the time came.
“This administration is notorious for poor planning. Look at the Department of Workforce Development debacle,” said state Rep. Joe Sanfelippo (R-New Berlin), chairman of the Assembly Health Committee, referring to the administration’s problems with settling thousands of unemployment claims. “This is just par for the course for them.”
What’s the administration’s vaccine distribution plan? The Wisconsin Department of Health Services has a “COVID-19 Vaccination Plan template” to assist with the development of a local jurisdiction’s COVID-19 vaccination plan.
“The template is divided into 15 main planning sections, with brief instructions to assist with content development. While these instructions may help guide plan development, they are not comprehensive,” the document states.
Recommended
A DHS official also pointed to the State Disaster Medical Advisory Committee (SDMAC) Vaccine Subcommittee. It was established to develop guidance for DHS to construct its plan for the distribution of the limited number of COVID-19 vaccine doses, especially in the first months following the vaccine release.
But the administration’s plan to deliver the vaccine to nursing homes is the federal government’s plan.
On Monday, the governor announced that DHS “officially activated” the federal government’s pharmacy distribution program for the COVID-19 vaccine.
“This announcement is another step forward toward ensuring our most vulnerable Wisconsinites get the vaccine quickly and safely,” Evers said in a statement, before the delayed distribution to nursing homes was made public.
Communication breakdown
Evers has said his administration has been preparing for some time in advance of the final federal approvals of a coronavirus vaccination. If so, he and DHS officials have not adequately communicated his plans to the Legislature and the general public, legislative sources said. Legislative offices told Empower Wisconsin this week that their constituents have said the lack of information from the governor’s office has left them confused about when they and their loved ones in long-term care facilities might expect to receive a vaccination.
“It seems like they don’t want to make an attempt to work with anybody other than themselves,” Sanfelippo said. “They have this inner circle they deal with, but they don’t talk to anybody else.”
On Wednesday, officials from the Wisconsin Department of Veterans Affairs weren’t sure when the vaccine would be distributed to the three state-run veterans homes. An official believes it would be the end of the month, but the details had yet to be finalized. She said nursing homes sent out a lot of information, some of it conflicting.
The U.S. Department of Veterans Affairs says it will provide vaccinations to front-line VA health care workers and Veterans residing in long-term care units in 37 of its medical centers across the country, including in Milwaukee, beginning this week.
Earlier this month, the governor sent a letter to the U.S. Department of Health and Human services asking that Wisconsin be prioritized ahead of other states in vaccine distribution. It was a political effort, mostly blaming the Wisconsin Supreme Court for checking his administration’s expanded pandemic powers.
“A significant contributor to the crisis we are facing is that most of our statewide mitigation efforts have been struck down, enjoined, or are currently the subject of ongoing litigation—including even a public health emergency declaration and order requiring face coverings in public places—and a legislature that has not convened in more than 230 days,” he wrote. “Consequently, while other states are experiencing similar surges, Wisconsin uniquely faces substantial barriers to implementing statewide mitigation strategies supported by public health experts and science currently utilized by other states.”
But the governor has had control of all of the money — $2 billion in federal COVID relief funding — and the flexibility to spend it how he sees fit in fighting the virus and its effects. That includes preparedness initiatives.
Complications
To be sure, there are myriad logistical complications involved in the rollout of a newly approved vaccine in the middle of a pandemic. John Sauer, president and CEO of LeadingAge Wisconsin, advocate for the state’s long-term care facilities, said a number of forces struck to delay distribution.
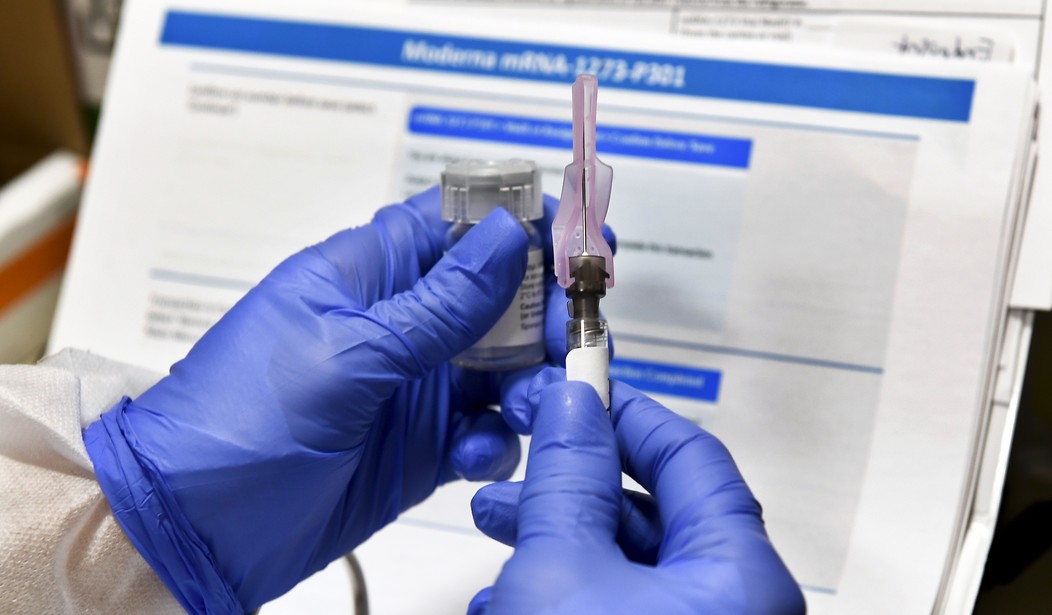
Pharmacy chains Walgreens and CVS originally planned to administer the Pfizer vaccine, but it must be stored at minus 94 degrees Fahrenheit, requiring special storage units and preparations. Most nursing homes don’t have those kinds of systems on site, so the Moderna vaccine, which doesn’t have to be kept in deep freeze, will be used instead. Moderna, as of Wednesday, was still waiting on FDA approval — expected to come any time.
Sauer said the delay is a concern but not unexpected given the massive distribution effort — 15,000 nursing homes nationwide.
Could the state have done more?
“I don’t know the answer to that question,” Sauer said. “As I have participated in a number of national and state preparedness calls, I do think there were a number of logistical issues where we might have been able to flip the switch to activate the program this week, but I think the end result would have been very few long-term care facilities would have received the vaccine.” There were less than 50,000 doses of the Pfizer vaccine available for distribution in Wisconsin this week.
DHS officials said Wisconsin could receive as many as 100,000 doses of the Moderna COVID-19 vaccine as early as next week. But vaccinations would not be available at nursing homes until after Christmas, as the pharmacy chains prepare and the care facilities seek consent from residents or their family members and representatives.
While the development, testing and approval of the vaccine has come at lightning speed, any delay in distribution is heartbreaking. Nursing homes have been hit particularly hard during the pandemic, more so in the latest surge of COVID-19 cases. DHS data show north of 2,000 residents and staff at Wisconsin’s nursing homes have been infected and more than 300 have died in the last two weeks.
“Every day that passes is a day where people who are more vulnerable to the virus are at greater risk,” said Sauer, noting that 91 percent of COVID-19-related deaths in the state are people 60 and over. The average age of nursing home residents is 85.
























Join the conversation as a VIP Member