Pfizer and Moderna just announced that in their advanced clinical trials, Covid-19 candidate vaccines have been 95 and 94.5 percent effective, respectively. Federal regulators could authorize the vaccines for emergency use within weeks -- and the public could start receiving shots before year's end.
That's amazing. If this timeline plays out, Pfizer and Moderna will win more than just the race to develop a Covid-19 vaccine. They will break the records for the fastest vaccine development by more than three years. And they couldn't have chosen a better time to do so.
Nor are Pfizer and Moderna the only game in town. Eight additional candidates are already in Phase 3 clinical trials, and altogether, 40 additional vaccine candidates are in development.
Every vaccine that proves safe and effective -- and can be made available at a reasonable cost -- is a gold medalist as there are 7.8 billion people on Planet Earth. That's a demonstrated demand for a lot of vaccine. In the Covid-19 Olympics, a successful vaccine plays every country's national anthem.
We're going to beat the pandemic because of pharmaceutical innovation.
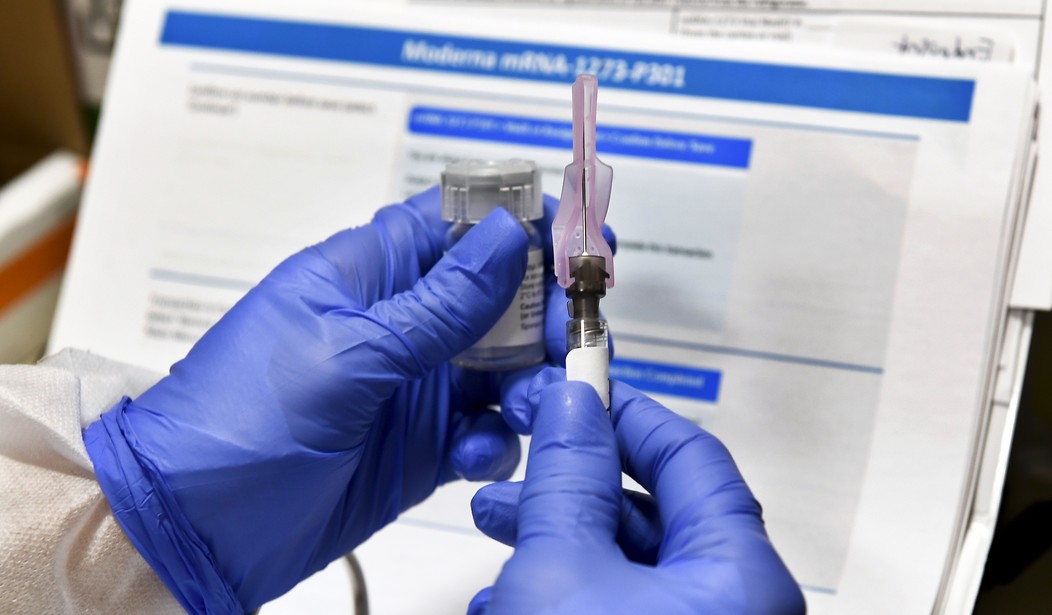
From the moment scientists first sequenced the genome of the novel coronavirus, research-based pharmaceutical companies leapt into action. Moderna's vaccine candidate moved to human trials just three days after President Trump declared a state of emergency. Pfizer was ready to move into final-stage trials by July.
Recommended
No one knew which, if any, vaccine candidate would succeed. But the ecosystem for private sector innovation has long been a powerful force in the United States in the development of breakthrough treatments and cures.
Pharmaceutical innovation is inherently risky. Less than 12 percent of promising compounds ever make it past clinical trials to market. Taking the inevitable failures into account, research and development costs for every success story run to the billions of dollars. A sound policy environment that promotes innovation has led to some of the most advanced research techniques of any industry -- just what we needed when Covid-19 came calling.
The federal government's Operation Warp Speed has identified several of the most promising vaccine candidates, including those from Pfizer and Moderna, and guaranteed government purchases in the billions of dollars for distribution to inoculate Americans and firmly contain the crisis and economic disruption. In Moderna's case and others, Operation Warp Speed has also contributed directly to funding for research and development.
But these federal investments would have been money wasted were it not for the technological capabilities and scientific know-how these research companies already had. New medications don't just involve the targeted compounds under investigation. Knowledge developed through laboratory and computer work often has multiple applications across many different investigations. Just because research doesn't pan out for the medical condition it was intended to treat, it doesn't mean it's a bust. Investigators, knowing its properties, can evaluate it for other conditions as well. Failure is the Father of Success.
Take for example, the first FDA approved coronavirus treatment, remdesivir. Gilead originally developed it in hopes of finding a treatment for hepatitis. That didn't pan out -- but Gilead did uncover its broad antiviral properties.
That was important news because the next work on remdesivir was as a treatment for the deadly tropical disease Ebola during the outbreak that began in West Africa in 2014. Again, no go. The National Institutes of Health (NIH) discontinued its remdesivir Ebola trial in 2018 after finding other treatments that were more effective.
But then came Covid-19. Researchers found that remdesivir could shorten hospital stays for those infected with the virus. It was the first major clinical breakthrough in developing treatments for those Covid-19 hits the hardest.
Today, as never before, the world needs innovation, and innovation requires a policy environment and market conditions that nurture it. That's what the United States brings to the table. Thanks to our brilliant scientists and our nation's free market economy, we are delivering relief from this pandemic faster than anyone could have imagined.
The research ecosystem is motivated as never before. Countless lives are at stake -- and probably a Nobel Prize or two.
Peter J. Pitts, a former Food and Drug Administration associate commissioner, is president of the Center for Medicine in the Public Interest.
























Join the conversation as a VIP Member