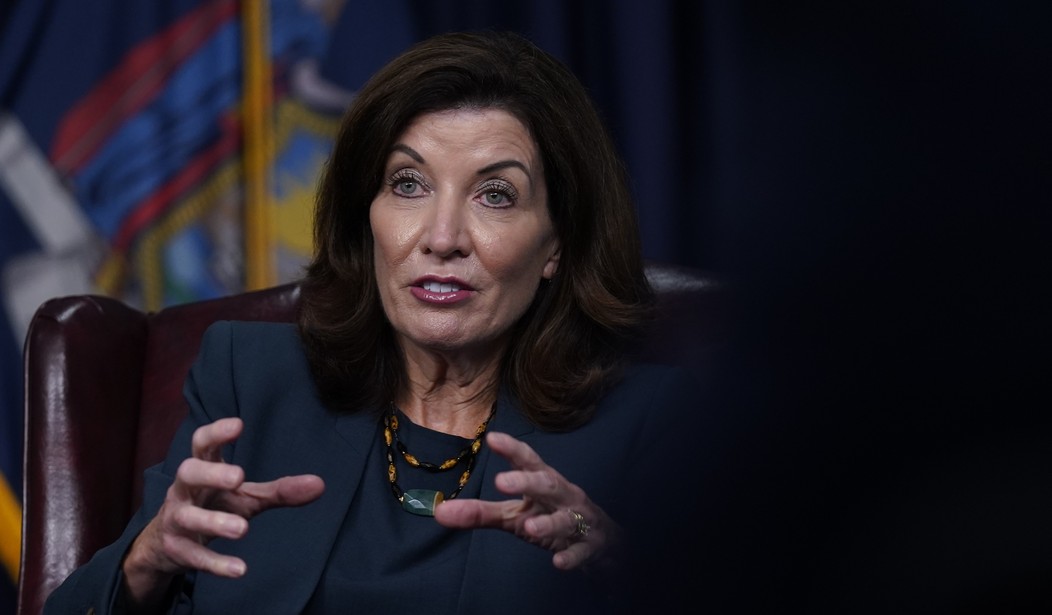
Over the weekend, New York Democratic Governor Kathy Hochul signed an executive order halting "elective" or "non-essential" surgeries in the state, claiming it was necessary to prepare for the arrival of the latest Wuhan coronavirus variant.
"We've taken extraordinary action to prevent the spread of COVID-19 and combat this pandemic. However, we continue to see warning signs of spikes this upcoming winter, and while the new Omicron variant has yet to be detected in New York State, it’s coming," Hochul released in a statement. "In preparation, I am announcing urgent steps today to expand hospital capacity and help ensure our hospital systems can tackle any challenges posed by the pandemic as we head into the winter months. The vaccine remains one of our greatest weapons in fighting the pandemic, and I encourage every New Yorker to get vaccinated, and get the booster if you’re fully vaccinated."
According to the New York Post, "the edict curbing non-essential surgeries will kick in for hospitals with a limited capacity — defined as at or below 10 percent of available staffed bed capacity" and will "take effect on Friday, Dec. 3, and will be re-evaluated based on the latest COVID-19 data on Jan. 15."
But "elective" surgery is subjective and oftentimes putting it off is life-threatening. In April 2020, Orthopedic surgeon Dr. Benjamin Domb explained the detrimental effects of halting surgeries last year.
While we remain focused on the urgent medical needs today, a secondary health care crisis is also brewing, and it threatens to be much larger than the crisis caused by the virus itself. It is the crisis of every other medical ailment that is being ignored, postponed or left untreated while we focus on coronavirus.
Federal and state governments have recommended a complete stoppage of all "non-urgent" procedures. Women cannot get annual mammograms. People with heart disease cannot get routine blood tests. Cancer screenings are becoming an afterthought. As a nation, we are in grave danger of pushing aside every aspect of medical care that is not related to COVID-19, and if we do not act quickly to balance our efforts, the conditions we are ignoring may incur a human cost that could far overshadow that of the virus.
As an orthopedic specialist, I'm seeing this come to life in my own practice. Just this week, I performed surgery on a vibrant, 28-year-old young man named Jeffrey who had fully torn his hamstring tendon.
A terrific former high school soccer player who still loves to play a variety of sports, Jeffrey was sidelined from all physical activity due to his injury. In the midst of this public health crisis, it took six weeks for him to get his MRI scan showing a significant tear, and longer yet to get referred to my care. If his surgery were delayed any further, his tendon tear would have become irreparable, and he would have suffered lifelong weakness and chronic pain.
Recommended
Further, new information shows limited access to hospitals during the pandemic has caused another health crisis. More people will die from late-stage cancer after lack of basic screenings. From the Radiological Society of America:
Significant decreases in CT imaging for cancer persisted even after the peak of the COVID-19 pandemic in 2020, delaying diagnosis and treatment and raising the possibility of more advanced cancers and poorer outcomes for patients in the future, according to a study being presented next week at the annual meeting of the Radiological Society of North America (RSNA).
For the new study, researchers from Massachusetts General Hospital (MGH) and Harvard Medical School in Boston compared cancer-related CT exams during three periods of 2020: the pre-COVID phase (January to mid-March), peak COVID (mid-March to May) and post-COVID peak (May to mid-November). They looked at CT volume and the type of care being delivered through imaging.
As expected, CT volumes dropped significantly during the COVID peak. CT for cancer screening fell a whopping 82%, while CT for initial workup, active cancer and cancer surveillance also saw significant declines. Volumes for cancer screening and initial workup failed to recover in the post-COVID peak period, remaining down 11.7% and 20%, respectively, from their pre-COVID numbers.
“The decline during the COVID peak was expected because of stay-at-home orders and the number of imaging departments that shut down as a precaution,” said study senior author Marc Succi, M.D., an emergency radiologist at MGH and executive director of the MESH Incubator, an in-house innovation and entrepreneurship center.
The persistence of the decline in CTs for cancer screening and initial workup likely means higher numbers of patients with advanced cancers in the future.
“We expect that we’re going to see increased morbidity and mortality due to the fact that these patients weren’t able to get their routine imaging,” Dr. Succi said. “You can also surmise that they probably didn’t have their routine elective follow-up appointments as well.”
























Join the conversation as a VIP Member