June marks Alzheimer’s and Brain Awareness Month. In the United States, nearly six million Americans are living with Alzheimer’s disease. Globally, more than 50 million people are currently afflicted with Alzheimer’s.
Alzheimer’s is a relentless disease that impairs memory and other central mental functions. Thankfully, there is finally a bit of hope that we could be closer to a cure for Alzheimer’s by way of a newly approved experimental drug.
The Food and Drug Administration (FDA) recently approved Biogen’sAduhelm(aducanumab), an experimental drug used to treat Alzheimer’s disease. This is the first Alzheimer’s treatment that has come to market since 2003.
Under the FDA’s Accelerated Approval Program (AAP), this treatment has been brought to market sooner than the traditional drug approval process would have ever allowed. In short, AAP applies to life-threatening or serious conditions. The drug manufacturers are still required to prove efficacy and show the drug provides clinical benefit. Furthermore, under AAP, the FDA maintains full control over the regulatory process and can make the determination that the drug must be pulled from the market if Phase 4 trials don’t go accordingly.
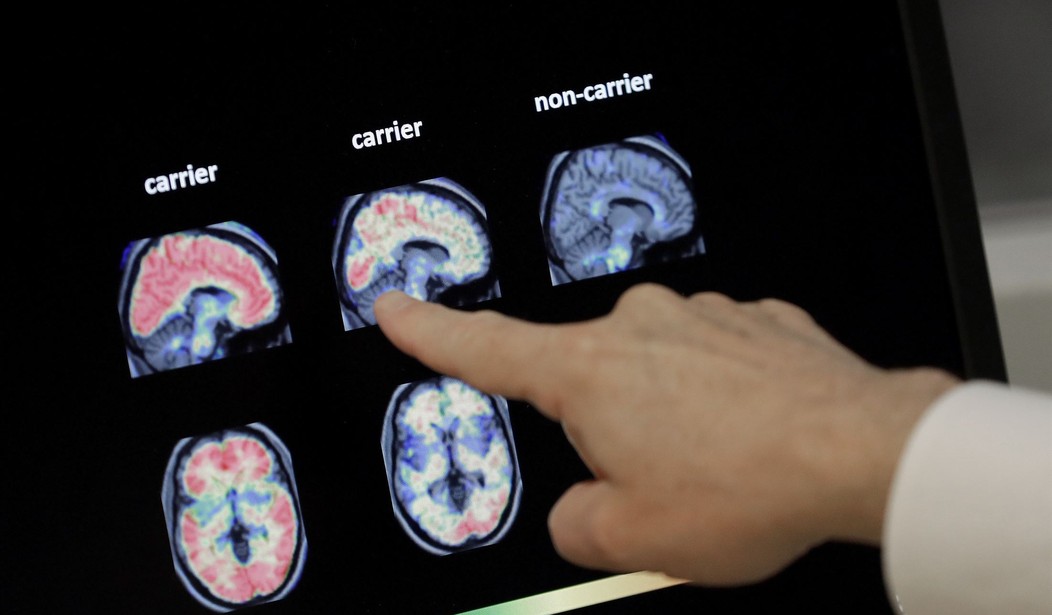
So far, patient advocates are cautiously optimistic about Aduhelm. Some data show the drug resulted in a reduction of clinical decline by reducing the level of amyloid plaques (sticky protein deposits) in the brain. The urgent push for access to this treatment is necessary because Alzheimer’s patients typically live at least four to eight years after diagnosis. Many patients live up to 20 years with this debilitating disease.
As is often the case, the good news also includes a bit of bad news. Several skeptics question the efficacy of the drug. Dr.Patrizia Cavazzoni, director of the FDA Center for Drug Evaluation and Research, recently opined that “there remains some uncertainty about the drug’s clinical benefit.”
Recommended
With that being said, the millions of patients (and their friends and families) suffering from this horrible disease deserve the chance to at least try a new medicine that could provide hope, if not help. After all, Alzheimer’s disease is the sixth leading cause of death in the United States. And patients deserve the right to try any and all treatments that could potentially save or improve their lives if they are suffering from a debilitating disease like Alzheimer’s.
On the health care legislative front, a new bill that was recently introduced in the U.S. Congress could improve the drug approval process to offer more treatment options for patients in the future. On June 3, Sen. Mike Braun (R-IN) introduced the Promising Pathway Act.
This bill aims to expedite approval of drugs for serious or life-threatening diseases, which would include Alzheimer’s. Currently, the FDA drug approval process typically takes 12 years and $2.9 billion to bring a drug from lab to market. This bill would improve FDA’s draconian drug approval process.
The COVID-19 pandemic has proved that expedited approval processes for lifesaving drugs can be extremely beneficial. The COVID-19 vaccines were approved for use after less than one year of research and development. There is absolutely no doubt that society has benefited from the expedited approval process granted to Operation Warp Speed.
Yet, this raises a bigger question: Why aren’t other potentially life-threatening treatments getting the same consideration? Biogen’s drug was recently approved via FDA’s AAP. However, it has been two decades since an Alzheimer’s treatment was granted full FDA approval.
Currently, 133 million Americans suffer from chronic illness. Nearly 40 percent of the U.S. population could benefit from an experimental treatment to battle their disease(s).
Without a doubt, Braun’s bill would be beneficial. If ever there was a piece of bipartisan legislation that Congress should pass, Braun’s bill is it. Allowing the FDA to establish a rolling, real-time, priority review pathway for necessary drugs that could save lives is a no-brainer.
We all want safe and effective drugs, but we don’t want overregulation that wastes time and money while millions of patients are waiting on their death beds for potentially lifesaving treatments. The goal is simple: cut costs and expedite approval of life-saving treatments for all diseases.
Christina Herrin is the government relations manager at The Heartland Institute, a nonpartisan, free-market think-tank headquartered in Arlington Heights, Illinois.
























Join the conversation as a VIP Member